Differential diagnosis rule number one: When you hear hoofbeats, think horses. In an ever-changing global environment and the severe consequence of a foreign animal disease introduction, we must always consider those hoofbeats could be from zebras.
This past October, 156 stakeholders, including representatives from the American Association of Swine Veterinarians, registered to attend the hybrid Japanese Encephalitis Virus (JEV) Symposium, hosted by the Center for the Ecology of Infectious Disease at the University of Georgia and sponsored, in part, by the Swine Health Information Center (SHIC). Stakeholders gathered to learn more about the Australian experience with JEV, discuss the known and unknown of JEV introduction and spread, and consider the potential animal and human health consequences if JEV were diagnosed in the United States.1
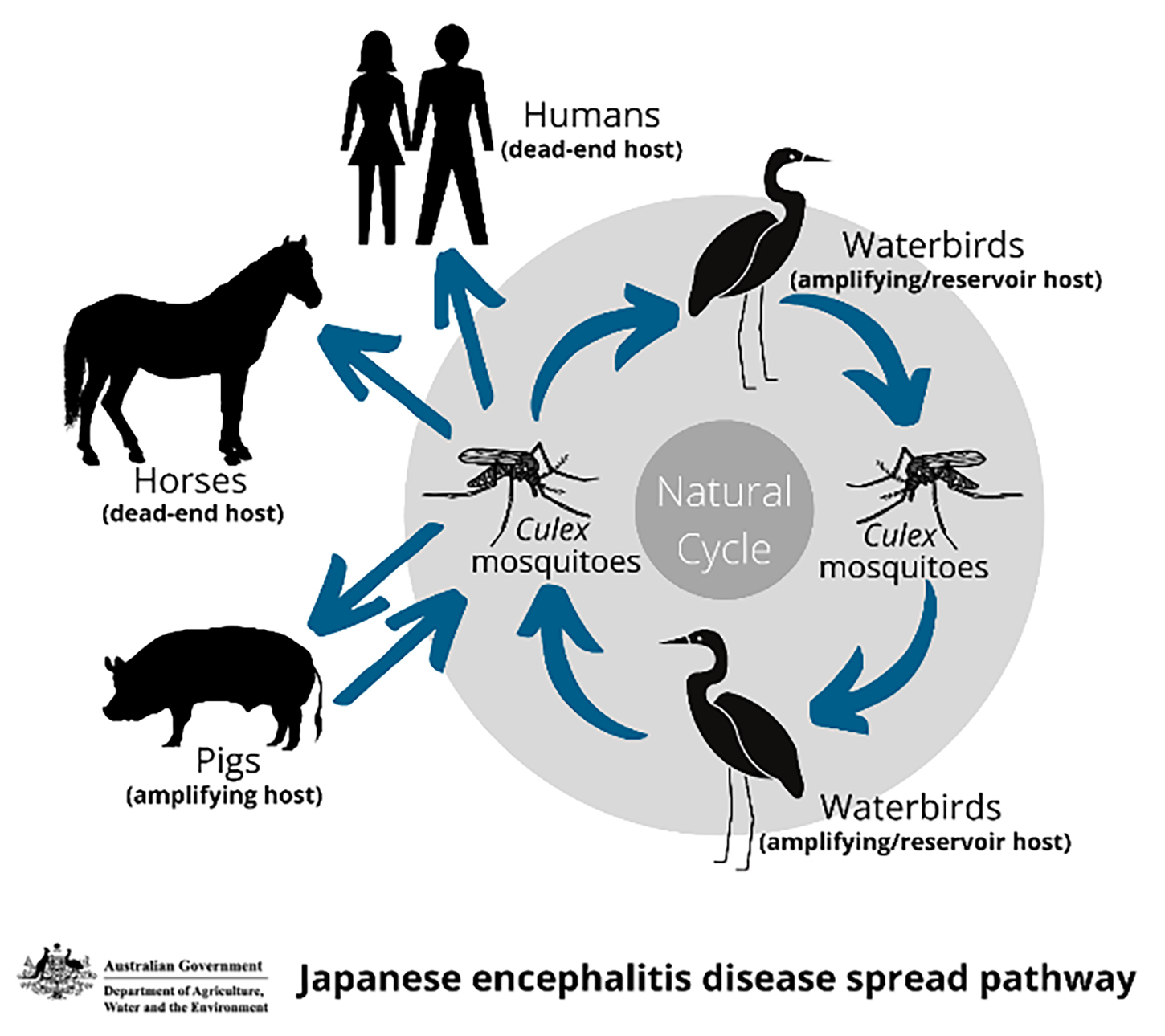
Japanese encephalitis virus is a zoonotic flavivirus in the same genus as dengue, yellow fever, and West Nile virus. It is transmitted primarily by the Culex mosquito species. Natural reservoirs include waterbirds from the Ardeidae family, such as herons and egrets. Clinical illness predominately occurs in equids, pigs, and humans; illness and asymptomatic infections have been documented in other species. Equids and humans are dead-end hosts while pigs are amplifying hosts.2
Dr Mark Schipp, Australia’s Chief Veterinary Officer, described 3 ways in which JEV might be detected. Animals or humans may present with clinical signs, or the virus may be identified through mosquito surveillance. In Australia, JEV was first diagnosed by multiple different veterinarians on different farms in different states simultaneously. It was subsequently identified in humans and mosquitoes.2
As with African swine fever, early detection of JEV and any other foreign animal disease relies on producers and veterinarians to react to and report anything out of the ordinary. During the 2022 JEV outbreak in Australia, swine veterinarians Drs Kirsty Richards and Bernie Gleeson observed delayed farrowing, reduced litter size, increased return to service, late term abortions, and mummified, stillborn, and shaking piglets.2
With these clinical signs, Dr Schipp cautioned of the likelihood of detection bias. Clinical manifestation of JEV may be noticeable in large sow farms, but it may be easily missed in smaller farms or when only a small percentage of animals is infected. In fact, JEV was likely circulating in Australia for at least 1 year before it caused a major outbreak in 2022.2
Dr Michael Neafsey, One Health Coordinator for the US Department of Agriculture’s Animal and Plant Health Inspection Service, also expressed concerns about delayed detection because of JEV’s nonspecific clinical presentation.3
JEV could have been introduced into Australia via migratory waterbirds, microbats or fruit bats, wind dispersed mosquitoes, or mosquitos in shipping vessels or aircraft. Previous risk assessments indicated aircraft and cargo ships as the most likely pathways for the introduction of JEV into the United States. Climate and geography likely impacted the sylvatic lifecycle and sustained transmission in Australia.2
Observed risk factors for JEV in Australian farms included the presence of standing water, water birds, and mosquitoes. Pig movement and semen movement, due to high quality control, did not seem to be risk factors.2
All presenters from Australia emphasized the importance of a One Health approach for a coordinated and efficient response. Dr Richards acknowledged time and resources spent on preparing for an African swine fever incursion was crucial to the JEV response. “It might not have been African swine fever that arrived, but nothing in that preparation was wasted. The work that we’ve done for African swine fever absolutely underpinned the collaboration we had with government during this response. We’ve learned that relationships, understanding, and credibility between government and industry stakeholders is pivotal to having a successful emergency disease response.”2
Further, Australian consumer impact was minimal largely in part because of messaging. The public was reassured that pork is safe, JEV is a mosquito-borne disease, and pigs are incidental hosts.2
A key action item from the symposium was to further educate swine veterinarians about JEV. In 2022, Dr Harry Snelson challenged veterinarians to report more often when things are unusual. “Everyone who sees pigs in the field must be empowered to raise the alarm when there are suspicions that things just aren’t normal.”4
Be vigilant, investigate every unusual health event, report anything different, and question the result.
There is still much to learn about JEV and its potential to impact human and animal health in the United States. If we can at least recognize the hoofbeats might be coming from a zebra, we will be ahead.
Presentations from the symposium have been archived and are freely available at ceid.uga.edu/jev2022/archive/.2 Additionally, information about the Australian JEV outbreak and response was featured in episode 10 of the SHIC Talk podcast (swinehealth.org/podcasts/) and the March 29, 2022 SHIC/AASV webinar (aasv.org/members/only/video/webinars/#v11).
Abbey Canon, DVM, MPH, DACVPM
Director of Public Health and Communications
References
*1. Sundberg P. JEV Symposium: Australian experience informs US preparedness. AASV. November 2, 2022. Accessed November 14, 2022. https://aasv.org/news/story.php?id=15233
*2. Symposium on Japanese Encephalitis Virus Emerging Global Threat to Humans & Livestock. University of Georgia Center for the Ecology of Infectious Diseases. October 17-19 2022. https://www.ceid.uga.edu/jev2022/
*3. Sundberg P. JEV Symposium: US preparedness underway. AASV. November 9, 2022. Accessed November 14, 2022. https://aasv.org/news/story.php?id=15277
*4. Snelson H. It’s probably nothing [Editorial]. J Swine Health Prod. 2022;30(4):207.
* Non-refereed references.